
Normal Retina
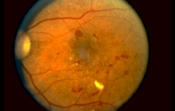
Diabetic Retina
What is Diabetes?
Diabetes affects 14 million Americans, though only about 7 million are aware that they have the condition. Most diabetics are Type II or non-insulin dependent diabetics, with fewer being Type I or insulin-dependent diabetics. Eye complication are more common as the duration of disease increases. After 20 years of diabetes, 99% of Type I diabetics and 60% of Type II diabetics will develop some degree of disease involvement in the retina. The retina, the most inner layer of the eye, functions like film in a camera. Light images are brought to a focus on the retina, which converts light signals into electrical signals transmitted through nerves to several areas in the brain. If the retina is not functioning properly, vision can be markedly affected.
What is Diabetic Retinopathy?
The exact mechanism of diabetic retinopathy is not yet fully understood. What is known is that continued high blood glucose (sugar) levels leads to damage to blood vessels throughout the body. Studies have shown that good control of glucose levels lowers the risk of retinal (and other) complications in all diabetics.
|
|
|
Diabetic retinopathy is classified into two stages. The earlier stage is called non-proliferative diabetic retinopathy. Non-proliferative retinopathy produces blood vessels changes within the retina: bleeding (hemorrhages), weakened blood vessel walls (microaneurysms), leakage of fluid (edema or exudate) and loss of circulation. Certain people with non-proliferative retinopathy may progress to proliferative retinopathy. This involves the development of new, fragile blood vessels with fibrous tissue on the surface of the retina. This condition can reduce vision as a result of bleeding from these fragile new blood vessels or by contraction of fibrous tissue.
How is Diabetic Retinopathy Diagnosed?
Diagnosis of diabetic retinopathy begins with a comprehensive
eye examination. A crucial part of this exam is dilation of the pupils with
special eye drops so that the entire retina can be examined. Photographs may be
taken of suspicious areas and additional testing such as fluorescein angiography
may be 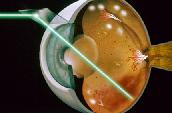 necessary
to determine whether and where abnormalities are present. Diabetic retinopathy,
when minimal, requires regularly scheduled eye examinations only. However, when retinopathy
worsens, more frequent examinations or laser treatment may be necessary. A
diabetic patient's ability to see well does not mean that the eyes are well.
Certain patients will have 20/20 vision and proliferative retinopathy requiring
treatment. Background retinopathy with leakage of fluid can often be improved by
limited laser treatment to the leaking blood vessels. In cases of more severe
bleeding into the eye or traction-related retinal detachments, surgery may be
necessary.
necessary
to determine whether and where abnormalities are present. Diabetic retinopathy,
when minimal, requires regularly scheduled eye examinations only. However, when retinopathy
worsens, more frequent examinations or laser treatment may be necessary. A
diabetic patient's ability to see well does not mean that the eyes are well.
Certain patients will have 20/20 vision and proliferative retinopathy requiring
treatment. Background retinopathy with leakage of fluid can often be improved by
limited laser treatment to the leaking blood vessels. In cases of more severe
bleeding into the eye or traction-related retinal detachments, surgery may be
necessary.
Diabetes may cause severe eye problems if left unchecked. Good control of blood glucose levels and comprehensive eye examinations annually are the best defense against vision loss.